Stop losing money to broken revenue cycles
END-TO-END, WORK-FREE RCM
The automation RCM & Prior Auth Platform for Telemedicine & Specialty Clinics
Stop managing fragmented vendors which operate like black boxes and let patients and revenue fall through the cracks. Foresight orchestrates everything from eligibility and prior auths to claims and denials. We use predictable, auditable rules custom-built for you + surgical AI automation + optional managed services for the edge cases automation cannot resolve. Tailored to your specific clinical area, medication mix, processes, and relationship with payers.
3 min to submission
92% 1-st pass rate
85% autohandled
3 min to submission 92% 1-st pass rate 85% autohandled
How it works
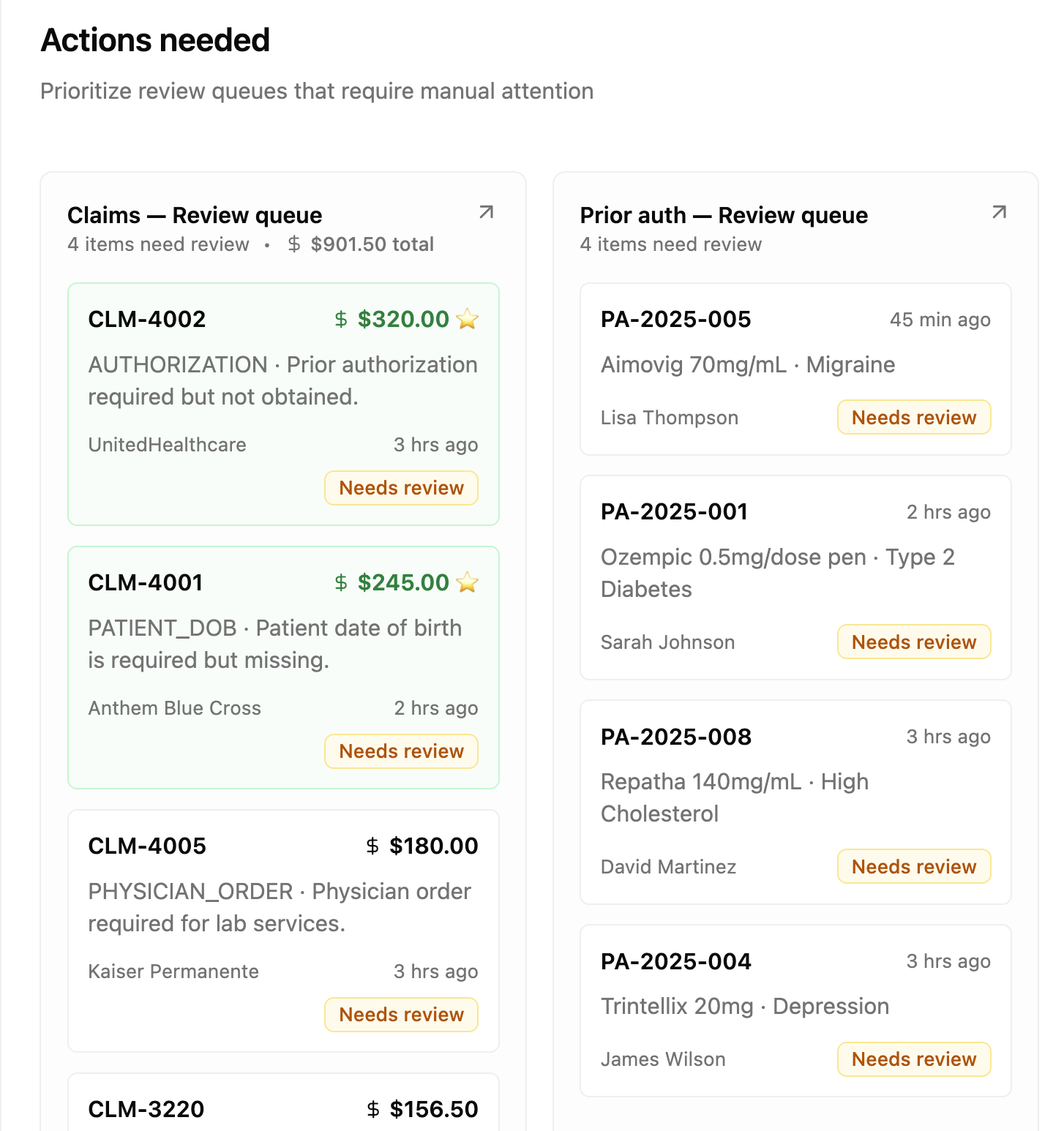
Prioritize what matters
Prioritize what matters
We do 85% automatically resulting in faster approvals overall, and guide humans on how to fix the remaining 15%
We automate most PAs and claims. Whenever we need a human to intervene we show them the specific items which truly need their attention, ordered by value, ready to take action.
Consolidated Workflow: Eligibility, PAs, and Claims in one view.
Smart Routing: We handle the complexity of TPAs and carve-outs so you don't have to.
Revenue Intelligence: Spot care gaps and under-utilized codes automatically to increase revenue per patient.
Clear actions
Clear actions
Targeted fixes + guardrails
We make seeing the specific fields that need fixing when human review is needed crystal clear and actionable. We hard-code predictable submission rules and use AI where strictly needed such as extracting missing ICD/CPT codes. We don't guess on eligibility or benefits; we execute logic you can audit
With you from start to scaling nationwide
With you from start to scaling nationwide
Built for High-Volume Care
Designed for digital health and specialty clinics managing complex workflows like GLP-1, TMS, or addiction. We handle the nuance of recurring visits, authorization limits, and specific documentation requirements that generic RCM tools miss
Custom-made for you
Custom-made for you
Built custom for you, priced as a product
The era when only the largest health systems could afford to build custom RCM solutions is over. We adapt our product and logic for each customer to deliver client-specific pipelines accommodating your data and relationship with payers, the analytics you need, etc
-
Every denied claim costs you $48 on average to rework
8% of your revenue disappears into billing complexity
Your best clinicians waste 2 hours daily on admin work
-
We use predictable, custom-built rules + AI only where needed to lift the workload of creating PAs or claims and submitting them off you. We integrate with all EHRs and submit claims and prior authorizations using clearinghouses, electronic prior auth APIs and prior authorization portals as needed for maximum coverage.
-
Other vendors promise AI magic. We deliver predictable revenue
Rules for what's certain (patient demographics, POS codes, time based E/M, etc.)
AI only where needed and when needed (e.g., ICD-10 and CPT codes)
Every decision traced and auditable
Submission and re-try playbooks per payer and clinical area
-
Turn denials from dead ends into dollars
We scan denial reasons to transform them into targeted fixes
E.g., CARC 197 → Missing auth → Auto-attach from ePA system → Resubmit → PAID
See denial patterns by payer, provider, while Foresight continuously learns and improves from past performance